Optic disc drusen, also known as hyaline or colloid bodies, are
hyaline, calcified, microbodies situated in the prelaminar part of the optic
nerve head1. The processes of development of drusen of the optic
nerve head is proposed as abnormal axonal metabolism leading to intracellular
mitochondrial calcification. Small calcified microbodies are formed and calcium
continues to deposit on the surface of these microbodies to form drusen2.
Axoplasmic transport variation is the anatomic substrate for creation of drusen
of the optic disk3. Optic
disc drusen are associated with shorter and
hypermetropic eyes, these anatomical situations and vascular factors may give
rise to pathogenesis of drusen4,5.
Optic disc drusen is present in 3.4 to 24 per 1,000 populations and are
bilateral in about 75%6. Optic disc drusen have irregular autosomal
dominant inheritance7. Because of continuous calcium deposition,
optic disc drusen will increase in size and will become more visible with age.
A correct diagnosis of optic disc drusen is compulsory, though effective
treatment is not yet present but it is most important to differentiate optic
disc drusen from papilledema in order to evade unnecessary neurological
examinations6,8. Clinical interpretations prove that the optic nerve head drusen are widely asymptomatic and that
visual acuity remains unaffected9 but discrete papillary
calcifications or hyaline bodies commonly emerge and visual field deficits are
commonly noticeable in the second decade of life in patients with
pseudopapilledema due to optic disc drusen10. This case is
presented to emphasize the importance of optic disc drusen and its association
with hypermetropia and inheritance.
CASE REPORT
12 year old male child and his 13 year old sister presented in
our eye outpatient department with decrease vision in both eyes since last 5
year. Both were student and had no systemic illness. General physical examination
and systemic examination were unremarkable.
Ophthalmologic examination of male child
revealed best corrected visual acuity with correction of +19.5 DS in both eyes
to be 6/60 (using Snellen’s visual acuity chart) with no pin hole improvement.
Best corrected visual acuity of female patient with correction of +19.0DS in
both eyes was 6/36 (using Snellen’s visual acuity chart) with no pin hole
improvement. There was no deviation in any eye and extra ocular muscle
movements were full in both eyes of both patients. Both pupils were round,
regular and reacting to light and no relative afferent pupillary defect was
noted. Biomicroscopic examination of both the anterior segments was
unremarkable. Fundoscopic examination showed bilateral blurred and swollen
optic discs margins with no hyperemia and with obliteration of the
physiological optic disc cupping (Fig 1A, 2A). Venous pulsations were present
in both
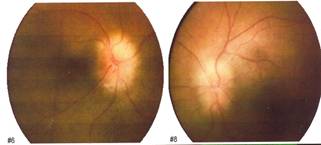
Fig. 1A
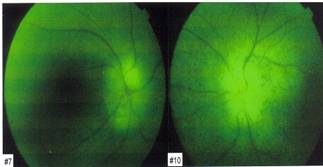
Fig. 2A: Fundus photographs of
patient showing bilateral optic disc swelling and blurred margins and obliteration
of the physiological optic disc cupping.
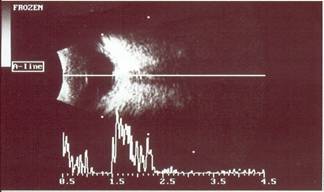
Fig. B: B-scan
ultrasonograph showing focal high acoustic reflectivity because of calcific
deposition.
eyes in both patients. Visual
field examination by confrontation showed grossly restricted peripheral visual
fields in both eyes but it was not possible to perform automatic Humphery
perimetry as the patients were young in age so were uncooperative and unable to
understand commands for automatic humphery perimetry. A diagnosis of bilateral
optic nerve head drusen was made, which was subsequently confirmed by B scan
ocular ultrasono-graphy (Fig B) and Optical Coherence Tomography (Fig C) in our
ophthalmic outpatient department. Additionally CT scan brain and orbit was done
to see the optic nerve head calcification and to exclude any central nervous
system pathology. Patients and their parents were informed about the condition
and cause of decrease vision, which was hypermetropia and their parents were
also informed that they and their other offspring should have an ophthalmic
examination to exclude optic disc drusens.
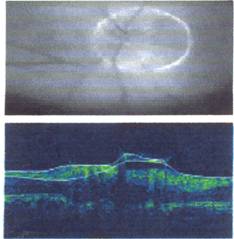
Fig. C: Optical
Coherence Tomography showing typically elevated optic nerve head and optically
empty cavity and perceptible reflection from posterior surface.
DISSCUSION
Optic disc drusen are congenital
and developmental anomalies of the optic nerve head
seen frequently in clinical practice, often as an incidental finding during
routine ophthalmic examination. Optic disc drusen can affect children as well
as adults. It is important to consider optic nerve head
drusen in the differential diagnosis of papilledema or optic nerve swelling in any age group11. The
primary pathology of optic disc drusen is an inherited dysplasia of the optic disc and its blood supply, which influence the
formation of optic disc drusen4,12.
Optic disc drusen has a greater tendency to form in eyes with a small scleral
canal; therefore hypermetropic eyes would have a higher rate of optic disc
drusen relative to myopic eyes5. The diagnosis of optic disc drusen
can be made with clinical findings combined with B scan ultrasound, Fundus fluorescein angiography,
Ocular computed tomography and newer modalities using optical
coherence tomography of optic nerve head,11 but ocular B-Scan
ultrasonography, a non-invasive and cost-effective technique is the most
sensitive and method of choice in the recognition of optic disc drusen8,13,15.
Optic disc drusen shows auto-fluorescence (ability
of substance to emit yellow-green light when stimulated by blue light in the
absence of fluorescein dye)
in Fundus fluorescein angiography. Incidental asymptomatic orbital
calcifications are frequently encountered on modern high-resolution CT scan
images of the brain and orbit14. Optical coherence tomography can
differentiate optic disc drusen from papilledema and small optic disc without
disc drusen as optic nerve head drusen typically
elevate the disc surface and appear as an optically empty cavity, sometimes
with a perceptible reflection from the posterior surface. The disc surface is
also elevated in cases of papilledema, but has a strong anterior reflection
behind which, there is no visible structure. The surface of the small optic nerves was slightly elevated, but with less
anterior reflectance,16 therefore OCT of optic nerve head exposed
unique and clinically helpful views of optic nerve drusen17.
The aim of presenting this case is that we
should consider optic disc drusen in any patient who presents with bilateral
optic disc swelling, particularly when the patient is hypermetropic and
asymptomatic.
CONCLUSION
In our case the unique feature is presence
of bilateral optic disc drusen in hypermetropic two children of the same
family. Optic disc drusen may be hereditary and have close association with
small scleral canal.
Author’s affiliation
Dr. Ghulam Mustafa Memon
Resident Medical Officer
LRBT, Free base
Korangi-2 1/2, Karachi-74900
Dr. Shakir Zafar
Consultant Ophthalmologist
LRBT, Free base
Korangi-2 1/2, Karachi-74900
Dr. Munira Shakir
Consultant Ophthalmologist &
Head of Pediatric Ophthalmology Department
LRBT, Free base
Korangi-2 1/2, Karachi-74900
Dr. Zeeshan Kamil
Ophthalmologist
LRBT, Free base
Korangi-2 1/2, Karachi-74900
Dr. Syeda Aisha Bokhari
Associate Opthalmologist
LRBT, Free base
Korangi-2 1/2, Karachi-74900
REFERENCE